hsv
Table of Contents
Herpes simplex virus (HSV)
patient information sheets
Introduction
- along with varicella-zoster virus, is a member of the neurotropic alpha group of the viral family herpetoviridae
- class 1, enveloped double-stranded DNA virus which replicates via their own DNA polymerase but use host RNA polymerase to build mRNA
- HSV usually causes local muco-cutaneous lesions at its point of entry then remains dormant within the local nerve cells until reactivated again resulting in episodes of painful vesicular lesions. HSV-1 may infect almost anywhere on the mucocutaneous part of the body, whereas HSV-2 has a preference for entry on genital labial surfaces.
- HSV-1 is mostly acquired in childhood, whereas HSV-2 is mostly acquired in adulthood as a sexually transmitted infection
- in most, the primary infection is asymptomatic whilst others will have a painful ulcerative condition, often with flu-like illness
- in some, the neural involvement may result in:
- Bell's palsy (usually HSV-1)
- encephalitis (usually HSV-1)
- aseptic meningitis (usually HSV-2)
- autonomic dysfunction of bladder, anal tone, etc. (usually HSV-2)
- referred neuropathic pain (usually genital herpes)
- chorioretinitis (neonates)
- it is the prime cause of erythema multiforme
- immunocompromised individuals are at risk of disseminated infection including pneumonitis, oesophagitis, hepatitis
Primary HSV gingivostomatitis:
- primary infection with HSV-1 is usually asymptomatic but in 20-25%, it presents as a herpetic stomatitis with many ulcers within the anterior aspect of the oropharynx in children aged 1-4 years. In adults it may present as a pharyngitis and probably accounts for about 5% of pharyngitis in university students.
- incubation period: median 6-8 days, range 1-26 days
- it is a self-limiting febrile condition lasting 10-14 days which requires only supportive care to prevent dehydration and to relieve pain.
- primary & recurrent HSV-1 lesions may occur almost anywhere such as fingertips (herpetic whitlow) and anywhere on wrestlers (herpes gladiatorum)
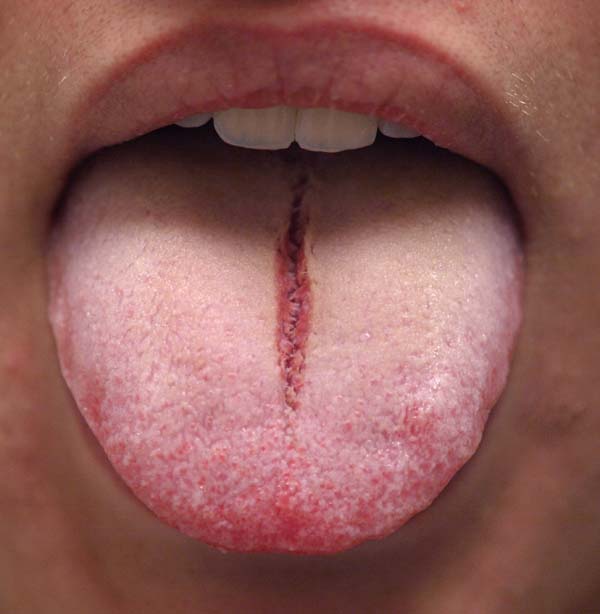
An unusual case of median tongue fissure in a teenager with otherwise classic primary HSV gingivostomatitis
Secondary herpetic stomatitis and cold sores (herpes labialis):
- recurrent episodes of HSV-1 stomatitis &/or cold sores typically around the mouth/nose but may occur elsewhere on the face
tends to occur in older children, adolescents and adults.
- people with underlying eczema may develop a more extensive form called eczema herpeticum or Kaposi's varicelliform eruption, not to be confused with dermatitis herpetiformis which is not caused by HSV but usually associated with an enteropathy such as coeliac disease.
- known precipitating factors include exposure to sun, cold, menstruation & fever.
- early topical aciclovir cream reduces severity and hastens resolution.
Herpes keratitis:
- primary HSV-1 ocular lesions occur in less than 5% of patients but may cause permanent corneal scarring or rarely, acute retinal necrosis.
- HSV-1 infection of the cornea is usually unilateral causing a foreign body sensation, redness, watery eye with variable decrease in visual acuity.
- slit lamp examination typically reveals branching dendritic corneal ulcers which are best seen on staining with flourescein or Rose Bengal stains.
Genital herpes:
aetiology:
- usually caused by HSV-2, but may be caused by HSV-1 virus (esp. female infants who have spread it by touch from their stomatitis or cold sore lesions or due to oral sex in adults).
prevalence:
- seroprevalence of HSV-2:
- 10-30% in Australians, lower in Asia, but nearly 70% in Kenya, Uganda, Zimbabwe (2003)
- estimated global prevalence of genital HSV-2 in young adults in 2020 was 17% in females and 10% in males 1)
- in contrast, estimated global prevalence of genital HSV-1 in young adults in 2020 was 10.5% in females and 9.9% in males 2)
- this also compares to the estimated global prevalence of oral HSV-1 in young adults in 2020 being 59% - higher prevalence in Africa while the Western Pacific had the largest number of infected individuals 3)
prevention of primary infection
- viral shedding is 100-1000x greater around periods of active lesions
- condom use may reduce risk of infection but certainly does not eradicate risk
- avoiding sex (including oro-genital and anal sex) during periods of recurrence in a partner (avoid for a week prior and after attacks if possible) also significantly reduces infection risk
clinical features
- primary infection may be very mild and unnoticed but also often results in:
- painful shallow genital ulcers lasting up to 3 wks
- tender groin lymphadenopathy
- pain and difficulty passing urine
- flu-like symptoms such as headache, fever, muscle aches may occur
- asymptomatic viral shedding is common and may occur a week before or after clinical recurrence
- stmptomatic recurrences most commonly cause very painful shallow ulcers of the labia or penis which last 5-10 days
- complications which may occur even without overt ulceration include:
- urethritis
- proctitis - fever, rectal pain, watery discharge
- autonomic nerve dysfunction with difficulty passing urine and possible acute urinary retention
- neuropathic pain referred to legs/thighs
- widespread infection may occur in debilitated patients
triggers for recurrence
- UV radiation (eg. sun)
- skin trauma
- pre-menstrual phase of cycle
- emotional stress
- other infections
diagnosis:
- swab for viral PCR
- serology :
- IgM response not diagnostically helpful as rise during recurrences as well as primary infection
- IgG response begin at 2-4wks after primary infection & present in virtually all by 12wks
- EIA type-specific gG1 & gG2 assays (available since late 1998, developed by Gull Laboratories):
- sensitivity & specificity 95-97% thus not good enough for low risk screening groups as false positive rates of 30% in pt with pre-test probability of only 10%
- potential indications:
- suspected HSV lesions where viral culture is negative or no lesions present at time of consult
- recurrent genital lesions thought to be non-herpetic but HSV needs to be excluded
- 1st episode - is it primary or recurrent
- asymptomatic partners to assess their risk of acquiring HSV-2 (debatable benefit as psychological problems may result)
treatment
- oral antiviral agents such as aciclovir may be used within 1st 72hrs to reduce duration and for those with frequent recurrences, can be used prophylactically
HSV-1 encephalitis:
- HSV encephalitis should be considered early in the presentation of acute neurological deficit, delirium or fever.
- it often mimics a variety of other conditions including stroke, delirium & sepsis.
- fever & headache are almost always present, while an altered level of consciousness may take hours or days to develop.
- focal neurologic deficits including aphasia, hemiparesis & visual field defects may occur, as well as behavioural changes, seizures or autonomic dysfunction.
- focal EEG changes are present in 80%.
incidence:
- 1:250,000 to 1:500,000 people per year
- mainly adults aged 40-70yrs - some cases are reactivation but most are genetically distinct secondary infection with entry probably via the olfactory system which would account for the typical distribution within the limbic system.
- NB. neonatal encephalitis is often due to HSV-2 which causes a more global encephalitic picture.
diagnosis:
- CSF PCR is the gold standard (98% sens, 100% spec) but may be negative before 2 days and after 10 days.
- CSF findings typically show mononuclear cell pleocytosis (present in 97% cases) with a mildly elevated protein & normal glucose. *CSF may be normal.
- CT findings:
- usually normal in 1st 2-3 days of illness & thus done to exclude other causes.
- early changes include low attenuation in the medial temporal lobes, insula & orbitofrontal regions with developing mass effect.
- MRI findings:
- may show changes within the 1st 2 days involving the limbic system.
treatment
- EARLY antiviral agents such as high dose iv aciclovir should be commenced in any patient with suspected encephalitis (fever, altered mental state, headache)
- supportive Rx
Disseminated neonatal HSV infection:
- neonates are particularly susceptible to vertical transmission of the HSV virus and infection may result in three main forms:
- localised to skin, eyes and mouth
- localised CNS disease causing encephalitis with a mortality of ~15% - neurologically normal outcome ~28% for HSV-2, >90% for HSV-1.
- severe disseminated disease with a mortality of over 50% which may also result in:
- chorioretinitis (posterior uveitis)
- fulminant hepatitis
- Initial symptoms can occur anytime between birth and four weeks. Patients with disseminated disease present earliest, often within the first week after delivery, while CNS symptoms usually occur during the second or third week.
- HSV is transmitted to an infant during birth, primarily through an infected maternal genital tract, although intrauterine infection may be a route of transmission
- the risk is greater with primary HSV infection acquired during pregnancy compared to reactivation of previous infection (35% versus 2%)
- among mothers with primary infection, acquisition near the time of labor is the major risk factor for transmission to the neonate.
- Transmission of infection appears to be substantially reduced by cesarean section (1.2% versus 7.7%).
- One problem with preventing neonatal HSV infection is that the diagnosis is not apparent in many mothers. In a national surveillance study of 184 cases, only 22 percent of mothers had a history of genital herpes and only 9 percent had genital lesions at the time of delivery.
Erythema multiforme
- HSV is the prime cause of erythema multiforme which is a delayed HS reaction to a HSV outbreak 7-10 days earlier which may be asymptomatic
hsv.txt · Last modified: 2024/12/13 03:43 by gary1